Advanced Solutions for Effective Parkinson’s Rehabilitation

According to the Parkinson’s Foundation, nearly 90,000 Americans receive a Parkinson’s disease (PD) diagnosis annually. Each diagnosis represents a patient and their loved ones facing a new reality that requires comprehensive support and innovative solutions. Parkinson’s rehabilitation that integrates exercise, biophysical agents, and innovative technologies can help these patients maintain independence and functionality longer.
Understanding Parkinson’s Disease
Parkinson’s disease is a progressive neurodegenerative disorder that impacts multiple aspects of movement and daily function. Patients often experience:
- Bradykinesia (slow movement)
- Muscular rigidity
- Resting tremors
- Shuffling and freezing gait
- Poor postural control
- Impaired balance
Exercise plays a key role in rehabilitation for this population, with additional benefits achieved by incorporating biophysical agents and rehabilitation technologies. Research demonstrates that exercise improves motor skill performance, which may be enhanced with cognitive engagement through feedback, cueing, dual-task training, and motivation.1 ACP provides several technologies that support this approach.
Virtual Reality Augmented Exercise

The American Physical Therapy Association recommends moderate- to high-intensity aerobic exercise for Parkinson’s patients to improve VO2, reduce motor disease severity, and improve functional outcomes. They also recommend resistance training to improve strength, power, nonmotor symptoms, and quality of life.2 Forced exercise with motor-assisted cycling has specifically been shown to improve motor function.3
OmniCycle Connect®, paired with the OmniTour™ Virtual Exercise Experience, can help Parkinson’s patients reap the benefits of aerobic exercise while providing cognitive engagement through immersive cycling and memory games.
Therapist considerations:
- Facilitate proper sitting posture throughout the activity.
- Consider interval training to allow higher intensity with less fatigue.
- Use forced cycling at a higher speed compared to a self-selected pace.
- Integrate biofeedback activities to provide visual/auditory cues, changes in speed/direction, and dual-task challenges.

There is also evidence that virtual reality rehab results in significantly greater improvement in balance and gait (BBS, TUG, and FGA) for Parkinson’s patients compared to conventional physical therapy.4
OmniVR® helps address patients’ cognitive impairment by incorporating activities that utilize memory and executive function. Through fun and interactive activities, patients are engaged and motivated to exercise harder and longer.
Therapist considerations:
- In the seated position, engage posture by varying support surfaces (firm, foam, balance ball).
- Vary speed with gait.
- Practice multi-directional movement.
- Progress to stepping over and avoiding obstacles.
- Perform squatting to facilitate picking something up from the floor.
E-Stim Enhanced Gait Training
Sensory electrical stimulation cueing during gait has been shown to reduce the time a patient needs to complete a walking task and the number of freezing gait episodes,5 which are common in many Parkinson’s patients.
The OmniVersa® Multimodality Therapy System’s Patterned Electrical Neuromuscular Stimulation (PENS) function can help re-establish normal muscle recruitment and firing, maximizing the benefits of regular gait training.
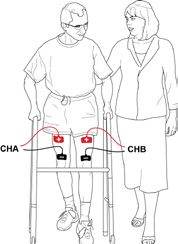
Therapist considerations:
- Use PENS UE and LE patterns to facilitate trunk and extremity exercise for improved posture control, strength, and coordination; apply during goal-oriented tasks when feasible.
- Use the PENS cycle or walk protocol to provide sensory/motor input to the CNS for gait initiation, symmetry, and cadence; vary the speed of the protocols.
Empowering Patients & Clinicians
Parkinson’s disease presents unique challenges and profound changes. By embracing innovative rehabilitation solutions, we can help these patients maintain their independence and quality of life longer.
Enhance Your Facility’s Parkinson’s Care
For more information on ACP technologies, explore our product suite.
- Petzinger, G. M., Fisher, B. E., McEwen, S., Beeler, J. A., Walsh, J. P., & Jakowec, M. W. (2013). Exercise-enhanced neuroplasticity targeting motor and cognitive circuitry in Parkinson’s disease. The Lancet. Neurology, 12(7), 716–726. https://doi.org/10.1016/S1474-4422(13)70123-6 ↩︎
- Osborne, J. A., Botkin, R., Colon-Semenza, C., DeAngelis, T. R., Gallardo, O. G., Kosakowski, H., Martello, J., Pradhan, S., Rafferty, M., Readinger, J. L., Whitt, A. L., & Ellis, T. D. (2022). Physical therapist management of Parkinson disease: A clinical practice guideline from the American Physical Therapy Association. Physical Therapy, 102(4), pzab302. https://doi.org/10.1093/ptj/pzab302 ↩︎
- Miner, D. G., Aron, A., & DiSalvo, E. (2020). Therapeutic effects of forced exercise cycling in individuals with Parkinson’s disease. Journal of the Neurological Sciences, 410, 116677. https://doi.org/10.1016/j.jns.2020.116677 ↩︎
- Feng, H., Li, C., Liu, J., Wang, L., Ma, J., Li, G., Gan, L., Shang, X., & Wu, Z. (2019). Virtual reality rehabilitation versus conventional physical therapy for improving balance and gait in Parkinson’s disease patients: A randomized controlled trial. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research, 25, 4186–4192. https://doi.org/10.12659/MSM.916455 ↩︎
- Rosenthal, L., Sweeney, D., Cunnington, A. L., Quinlan, L. R., & ÓLaighin, G. (2018). Sensory electrical stimulation cueing may reduce freezing of gait episodes in Parkinson’s disease. Journal of Healthcare Engineering, 2018, 4684925. https://doi.org/10.1155/2018/4684925 ↩︎
MRK-BLOG-023
According to the Parkinson’s Foundation, nearly 90,000 Americans receive a Parkinson’s disease (PD) diagnosis annually. Discover how exercise, biophysical agents, and innovative technologies can help these patients maintain independence and functionality longer.
Latest Updates
Subscribe to stay up-to-date on our latest posts.