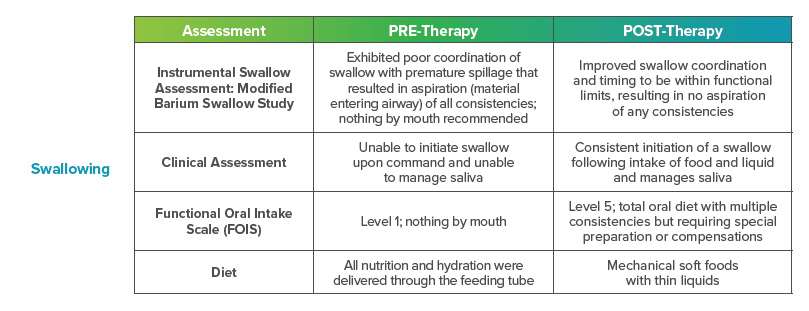
After undergoing coronary artery bypass graft (CABG) surgery, a 78-year-old gentleman faced a difficult recovery that impacted his voice and speech. Multiple falls left him vulnerable, and his most recent fall resulted in a head injury that required hospitalization and a referral to a skilled nursing facility for rehabilitation.
The patient expressed concerns that his voice and speech had changed after his fall, which was negatively impacting his ability to engage socially. Due to these concerns, he was evaluated by speech-language pathologists and referred to speech therapy.
Therapy Protocol
Speech Therapy
- 3x/week x 4 weeks
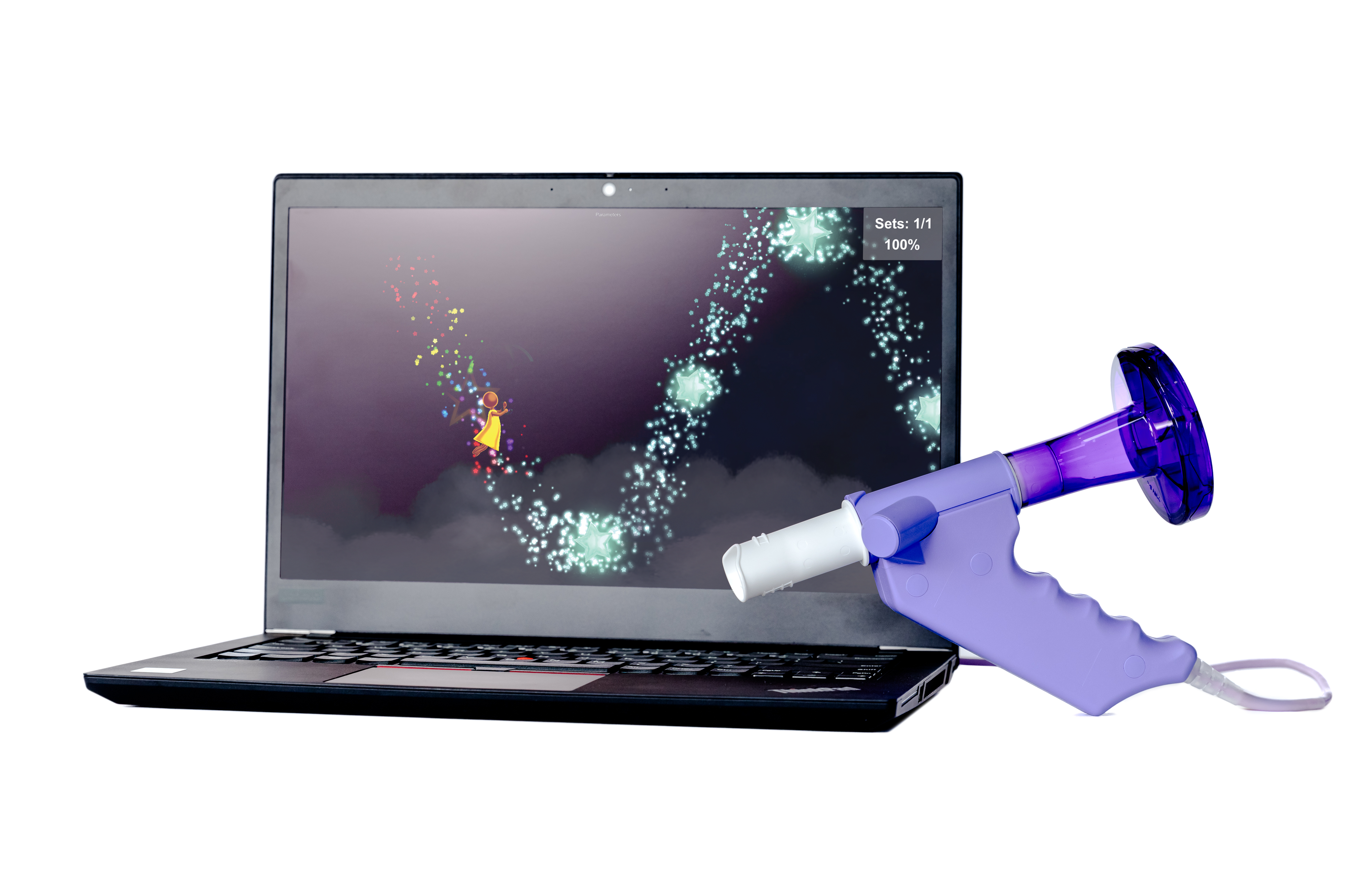
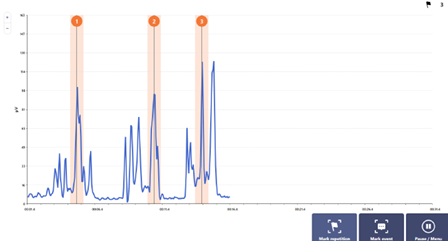
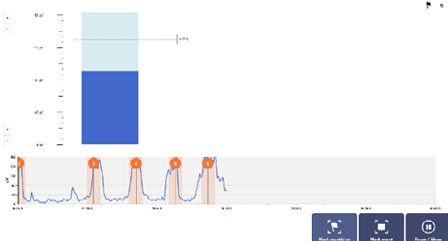
OmniFlow® Breathing Therapy Biofeedback System
- Controlled inspiratory lung volume – Diamond Mine
- Forced expiratory lung volume – Prehistoric Contest
Patient Education
- Good vocal hygiene to improve vocal quality
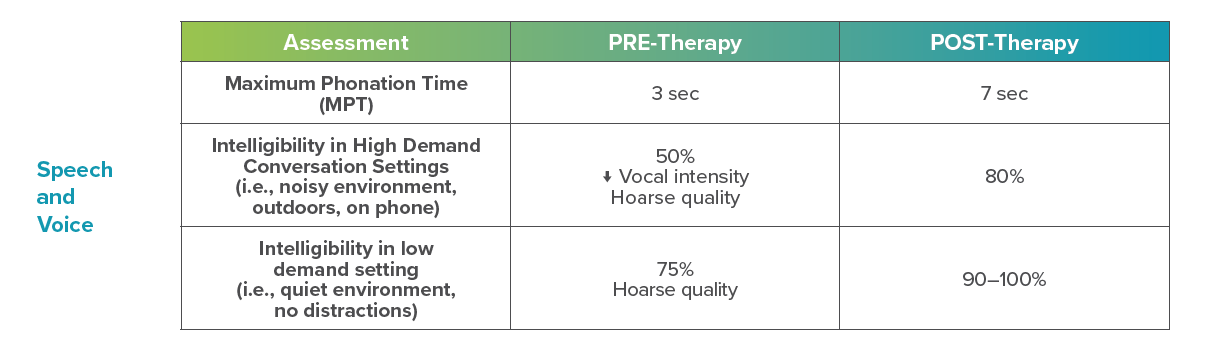
The patient and his significant other were happy that through therapy, he was able to regain his confidence and clarity of speech. The patient was able to engage in social activities he had avoided, such as talking on the phone, speaking around others at the rehab gym, and conversing with unfamiliar people.
I found having the graphics and game-like aspect vs. numbers on a screen very useful and positive. I feel it was challenging to me and helped my lungs expand to help with my voice.
Patient
Bring the OmniFlow® Breathing Therapy Biofeedback System to your Facility
Make speech therapy more interactive, engaging, and confidence-building for your patients with the support of virtual reality.
After a serious heart surgery and multiple falls, this 78-year-old patient found himself struggling not only with physical recovery but also with changes to his voice and speech that made social interactions difficult. In our latest blog post, we share how his care team used OmniFlow to help him regain his voice and confidence.
MRK-BLOG-033