Rising compliance costs, staffing shortages, and tighter reimbursement are reshaping the skilled nursing landscape heading into 2026. Our latest industry outlook breaks down the key pressures and strategic moves facilities are making to stay financially and clinically strong.
OBRA and Medicaid Advantage: Financial Compression Intensifies
The Omnibus Budget Reconciliation Act (OBRA) requirements and the growing influence of Medicaid Advantage plans are creating what experts call “compression on both sides of the ledger.” Compliance costs are rising as facilities adapt to new staffing and quality mandates, while reimbursement rates remain tight under managed care contracts. This dual pressure forces providers to rethink operational strategies, streamline workflows, and explore alternative revenue streams such as outpatient therapy or specialized programs. Financial agility will be critical for survival in 2026.
Persistent Staffing Pressures
Despite CMS rescinding a specific number of hours for RN staffing in skilled nursing facilities (SNFs), staffing remains the most significant challenge. OBRA’s staffing mandates add complexity, requiring facilities to meet minimum standards while managing wage inflation and a shrinking labor pool. According to HRSA workforce projections, demand for nursing professionals—including registered nurses and licensed practical nurses—will continue outpacing supply through 2026. The shortage is particularly acute in long-term care settings, where turnover rates remain high. Providers are responding with creative retention strategies, including flexible scheduling, career development programs, and technology-driven workforce management tools. The ability to attract and retain skilled caregivers will directly impact quality ratings and reimbursement, making workforce stability a top priority.
Occupancy Rates Rebound
After years of pandemic-related declines, occupancy rates are finally climbing back. This “great census rebound” offers a much-needed boost to revenue, but it also brings new challenges. Higher census levels increase pressure on staffing and resources, requiring providers to scale operations efficiently. Facilities that can balance occupancy growth with quality care delivery will be best positioned to capitalize on this trend. For many operators, this rebound represents a turning point toward financial recovery.
Value-Based Care and Medicaid Advantage Growth
Medicaid Advantage plans continue to accelerate the shift toward value-based care models. Contracts increasingly tie payment to quality metrics, patient outcomes, and readmission rates. SNFs must invest in data analytics and care coordination to meet these benchmarks and avoid penalties. Those who embrace value-based strategies will not only secure better payment but also strengthen relationships with payers and referral sources.
In 2026, star ratings aren’t just a quality metric—they’re a financial lifeline. Higher ratings mean stronger Medicare share and better margins: 5-Star facilities average 2.6% operating margins versus just 0.4% at 1-Star. They also gain more referrals from hospitals and Medicare Advantage plans, widening the gap even further.
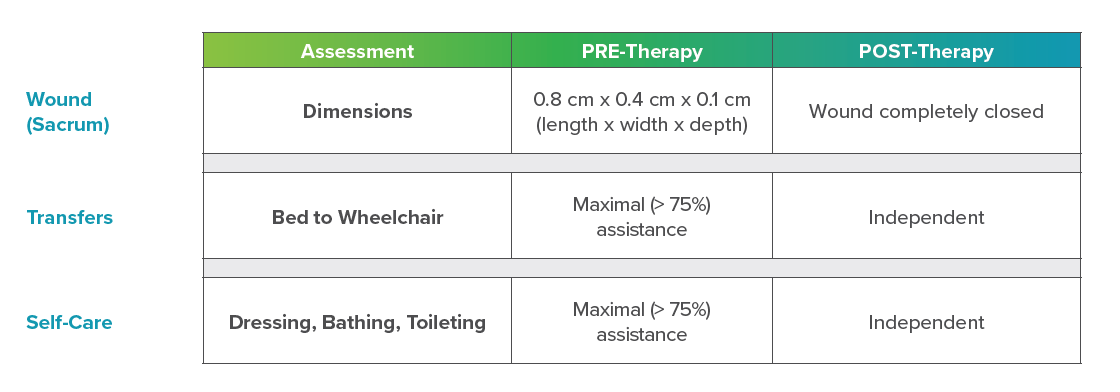
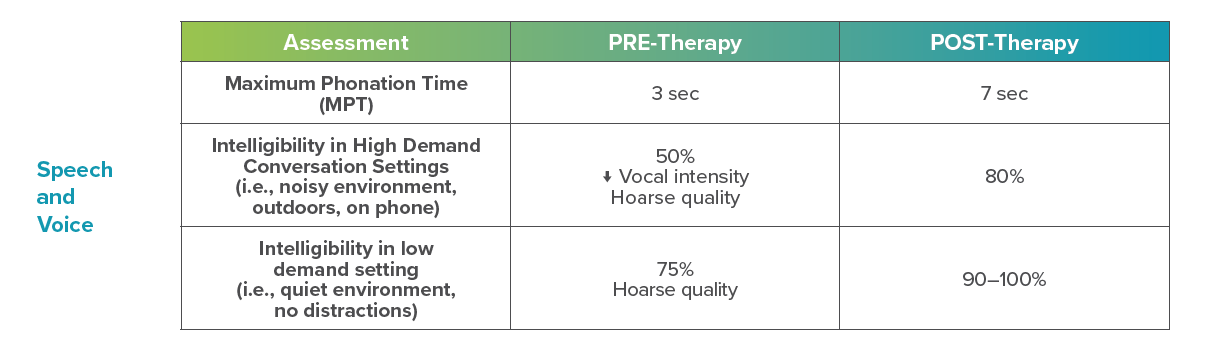
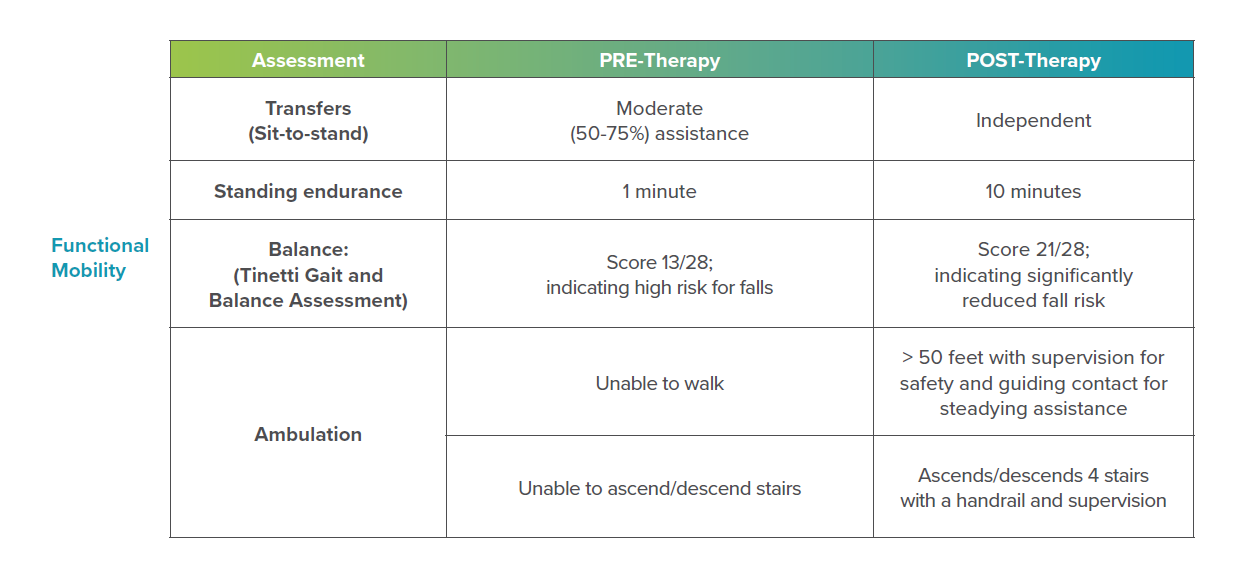
Improving star ratings is essential for sustainability—and ACP can help. Independent data shows our evidence-based clinical programs deliver superior functional outcomes and higher quality measure ratings compared to non-ACP customers. Partnering with ACP positions your facility for better care, stronger ratings, and greater financial success.
Strategic Partnerships and Diversification
To mitigate financial risk and expand service offerings, SNFs are forming partnerships with home health agencies, outpatient providers, and even acute care hospitals. These collaborations create integrated care networks that improve patient transitions and open new revenue streams.
According to McKnight’s 2026 Outlook, providers are increasingly leveraging these partnerships to strengthen referral pipelines and enhance continuity of care. Similarly, Skilled Nursing News reports that diversification beyond traditional SNF care—such as adding outpatient therapy or home health services—will be a key growth strategy in 2026 as operators seek to offset reimbursement pressures and capture new market opportunities.
Looking Ahead
2026 will be a year of adaptation and innovation. Providers who embrace technology, strengthen compliance, and align with value-based care will be best positioned to thrive.
At ACP, we’re committed to helping you succeed in this evolving landscape. By combining advanced clinical programs, innovative technologies, and expert education, we empower providers to deliver superior outcomes and elevate their quality of care. Together, we can transform challenges into opportunities and build a future where patients and providers thrive.
Your Partner in Better Patient Outcomes
Interested in learning more about how ACP can support your facility’s success in 2026?
CONTACT US
MRK-BLOG-036