Stroke is a debilitating condition that can cause significant muscle weakness throughout the body, including the muscles responsible for respiration. This can severely impact a patient’s ability to perform daily activities. Respiratory dysfunction occurs in 60% of stroke cases—what’s more, research has found an association between post-stroke apnea and cognitive decline.1 Fortunately, innovative devices like the ACPlus® Respiratory Assessment (ARA) and OmniFlow® Breathing Therapy Biofeedback System are designed to proactively identify and address these respiratory issues, enhancing recovery and improving quality of life for stroke patients.
Proactively Identifying Breathing Issues with ACPlus® Respiratory Assessment (ARA)

Stroke-induced respiratory dysfunction (SIRD) is associated with a higher 1-year mortality rate and worse functional outcomes, making it critical to catch as early as possible. ACPlus Respiratory Assessment (ARA) is uniquely designed to help clinicians proactively identify undiagnosed respiratory deficits. A clinician can conduct breathing tests that capture baseline metrics using an iPad and Bluetooth spirometer. ARA interprets that data to suggest possible lung disease patterns and severity levels. The clinical team can then use that data to develop the best treatment plan for that patient.
Delivering Targeted Interventions with OmniFlow®
Once respiratory deficits are identified, targeted interventions can be initiated. The OmniFlow Breathing Therapy Biofeedback System offers a variety of engaging exercises designed to improve respiratory muscle function, including:
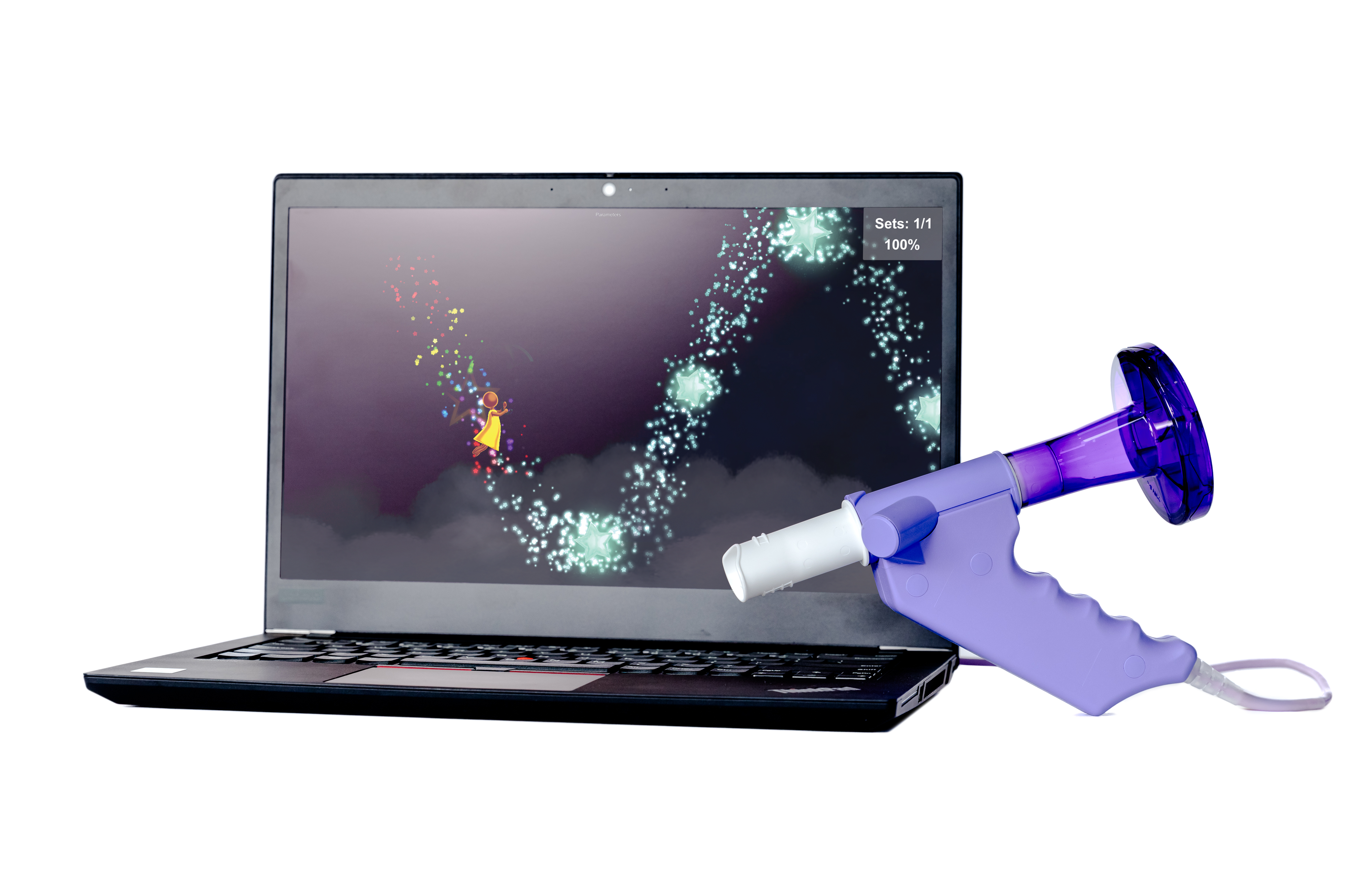
- Rhythmic Breathing: Focuses on rhythmical inspiratory and expiratory breathing
- Deep Inhalation: Improves inspiratory muscle power and inspiratory vital capacity (IVC)
- Forced Expiration: Targets expiratory muscle power
- Controlled Expiration: Improves controlled expiratory volume and flow
- ACBT/Huff Technique: Teaches patients the Active Cycle of Breathing (ACBT)/Huff technique to clear secretions from the lungs
OmniFlow provides valuable inhalation and exhalation data, helping clinicians better assess the patient’s condition and guide their treatment accordingly.
Benefits of Breathing Therapy Post-Stroke
Incorporating clinically appropriate breathing therapy into post-stroke rehabilitation offers numerous benefits. Respiratory muscle training effectively improves pulmonary function, strength of expiratory and inspiratory muscles, and walking ability, which can help patients perform daily activities more efficiently.2 Better respiratory control can also reduce the risk of complications like pneumonia. Including innovative tools like ARA and OmniFlow in treatment plans can help stroke patients recover faster and more effectively.
Enhance Your Respiratory Rehabilitation
For information on bringing ARA and OmniFlow to your patients, contact our team today.
- 1. Patrizz, A., El Hamamy, A., Maniskas, M., Munshi, Y., Atadja, L., Ahnstedt, H., Howe, M., Mulkey, D., McCullough, L., & Li, J. (2023). Stroke-induced respiratory dysfunction is associated with cognitive decline. Stroke, 54(7), 1863-1874. https://doi.org/10.1161/STROKEAHA.122.041239 ↩︎
- 2. Pozuelo Carrascosa, D., Carmona-Torres, J.M., Alberto Laredo-Aguilera, J.A., Pedro Ángel Latorre Román, P.A., Párraga Montilla, J. A., Cobo-Cuenca, A.I. (2020). Effectiveness of respiratory muscle training for pulmonary function and walking ability in patients with stroke: A systematic review with meta-analysis. International Journal of Environmental Research and Public Health, 17(15), 5356. https://doi.org/10.3390/ijerph17155356 ↩︎
MRK-BLOG-025
Did you know that respiratory dysfunction occurs in 60% of stroke cases? What’s more, research has found an association between post-stroke apnea and cognitive decline. Fortunately, innovative devices like the ACPlus Respiratory Assessment (ARA) and OmniFlow Breathing Therapy Biofeedback System are designed to proactively identify and address these respiratory issues, enhancing recovery and improving quality of life for stroke patients.